As the US slowly recovers from the devastating COVID-19 pandemic, a significant shift is underway in the scientific community. Just as the nation is learning to adapt to a post-pandemic reality, the National Institutes of Health (NIH) is making a notable decision that has left many researchers and experts wondering about the future of COVID-19 research. In a move that has sparked debate and curiosity, the NIH has announced plans to significantly cut funding for COVID-19 research projects, effectively signaling the end of an era for pandemic-related studies. But what does this mean for the scientists working tirelessly to combat the virus, and what are the implications for our understanding of this once-fearsome foe?
The Urgency of Preparation
The recent COVID-19 pandemic has highlighted the need for rapid response and preparedness. Pandemics are unpredictable and can spread quickly, causing significant harm and loss of life. The importance of investing in research to develop universal vaccines and treatments cannot be overstated.
According to NIH Research Matters, pandemics are unpredictable and can spread quickly, causing significant harm and loss of life. The recent COVID-19 pandemic, caused by a previously unknown coronavirus called SARS-CoV-2, seeded outbreaks across the globe in record time. By the end of 2022, it had killed more than 6 million people worldwide.
But COVID-19 was far from humanity’s first pandemic. As recently as 15 years ago, an outbreak of pandemic flu sickened 60 million people globally. In 2003, a new disease called severe acute respiratory syndrome, or SARS, sickened more than 8,000 people worldwide. It was caused by a virus called SARS-associated coronavirus (SARS-CoV).
No one can predict when the next pandemic will happen—only that one eventually will. These recent pandemics have brought into stark relief the need to be prepared for the next emerging disease, whenever it arrives. To this end, NIH-funded research teams have been working to develop universal vaccines against diseases with pandemic potential.
Research in Context: Progress toward universal vaccines
UW Medicine Institute for Protein Design In March 2020, the world changed in the blink of an eye as countries around the world locked down to slow the spread of COVID-19. This often deadly disease, caused by a previously unknown coronavirus called SARS-CoV-2, seeded outbreaks across the globe in record time. By the end of 2022, it had killed more than 6 million people worldwide.
But COVID-19 was far from humanity’s first pandemic. As recently as 15 years ago, an outbreak of pandemic flu sickened 60 million people globally. In 2003, a new disease called severe acute respiratory syndrome, or SARS, sickened more than 8,000 people worldwide. It was caused by a virus called SARS-associated coronavirus (SARS-CoV).
No one can predict when the next pandemic will happen—only that one eventually will. These recent pandemics have brought into stark relief the need to be prepared for the next emerging disease, whenever it arrives. To this end, NIH-funded research teams have been working to develop universal vaccines against diseases with pandemic potential.
Moving beyond educated guesses
For some viruses, the only constant is change. Locked in a continuous battle with the human immune system, many common viruses change, or mutate, rapidly. This means that even if you’ve been infected with a previous version of a virus, your immune system may not recognize an altered version the next time around.
A well-known example of the arms race between viruses and humans is the influenza virus, commonly known as the flu. More than 20 types of the virus—each of which, in turn, contains many different strains—circulate among people and animals, changing almost constantly.
The flu vaccine you get every year targets four strains that the scientific community predicts are most likely to predominate that season. “We have a well-established system to collect [information] on which strains are circulating all over the world,” says NIH vaccine researcher Dr. Karin Bok. “But it takes at least six months from the decision of which [strains] to include to the vaccine being available to the public.”
And which flu strains circulate during that time can change unpredictably. As a result, seasonal flu vaccines vary in their effectiveness. Their ability to prevent severe disease ranges from as high as 60% to as low as 10%.
All widely used flu vaccines to date teach the immune system to recognize a protein called hemagglutinin, which is found on the surface of the influenza virus. The virus uses hemagglutinin to enter human cells.
Recent NIH-funded study
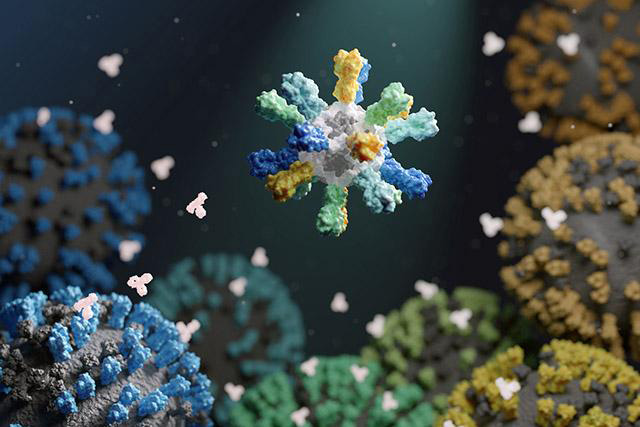
In a recent NIH-funded study, researchers designed a flu vaccine to provide broad protection against different influenza viruses. To create the vaccine, the researchers fused hemagglutinin to building blocks that assemble into nanometer-sized particles, or nanoparticles. The nanoparticles included hemagglutinin from four different flu strains.
The researchers reasoned that this would encourage the immune system to respond to parts of the protein that are shared across different strains of the virus. This approach could potentially lead to a universal flu vaccine that protects against all influenza viruses, regardless of their specific strains.
- This research could have significant implications for public health, as it would provide a way to protect against future pandemics.
- The development of a universal flu vaccine would be a major breakthrough in the fight against infectious diseases.
The Challenge of Mutating Viruses
The battle between pathogens and human immunity is an ongoing arms race. Viruses, such as the influenza virus and SARS-CoV-2, continuously mutate, leading to new strains that can evade the body’s immune defenses. This dynamic presents a formidable challenge for public health measures, particularly in the context of vaccine development and effectiveness.
As exemplified by the influenza virus, which undergoes frequent genetic changes, the efficacy of seasonal flu vaccines can vary widely from year to year. According to the CDC, the effectiveness of the flu vaccine in the 2019-2020 flu season was only around 45%, while in the 2017-2018 season, it reached an impressive 62%. These fluctuations are largely due to the virus’s ability to alter its surface proteins, making it difficult for existing vaccines to provide consistent protection.
One of the key proteins targeted by flu vaccines is hemagglutinin. This protein is critical for the virus to attach to and enter host cells. However, the constantly evolving nature of hemagglutinin means that the vaccine’s effectiveness can diminish as new strains emerge that are not covered by the existing vaccine. This underscores the importance of developing vaccines that can adapt to these mutations and offer broader protection.
The impact of viral mutations on vaccine effectiveness is a significant concern for public health officials. The NIH, in its quest to mitigate the effects of future pandemics, is focusing on the development of more adaptable vaccines that can target conserved elements of a virus, thereby providing a wider range of protection against different strains.
Universal Vaccines: The Future of Pandemic Prevention
The Concept of Universal Vaccines
Universal vaccines represent a paradigm shift in the way we approach vaccine development. Unlike traditional vaccines that target specific strains of a virus, universal vaccines aim to train the immune system to recognize and combat a broad spectrum of viral strains, including novel and emerging ones. This approach seeks to address the limitations of current vaccines that often have to be reformulated each year to match the circulating strains of a virus like influenza.
The concept hinges on identifying and targeting conserved regions of viruses that remain stable across different strains. By focusing on these stable elements, universal vaccines can potentially offer long-lasting protection against a wide array of pathogens. This is particularly critical for viruses like influenza, which undergo frequent mutations, rendering seasonal vaccines less effective.
Challenges in Developing Universal Vaccines
The development of universal vaccines faces significant hurdles. One of the primary challenges is the identification of stable targets on the virus that do not mutate significantly between strains. Hemagglutinin, for instance, is a prime target for the influenza virus, but its high mutation rate makes it a difficult candidate for a universal vaccine. Researchers must find parts of the virus that remain constant even as other parts evolve rapidly.
Another challenge is the complexity of the immune system’s response to these conserved elements. For a vaccine to elicit an effective and long-lasting immune response, it must engage with the immune system in a way that promotes the development of memory cells capable of recognizing and neutralizing multiple strains of a virus. This requires a deep understanding of immunology and the specific mechanisms by which vaccines can best harness the immune system’s power.
Recent Advances and Potential Impact
Despite these challenges, recent advancements in vaccine technology have brought the development of universal vaccines closer to reality. One promising approach involves the use of nanoparticle-based vaccines. In a study published by the NIH, researchers used nanoparticle technology to present multiple copies of hemagglutinin from different influenza strains. The nanoparticles were designed to mimic the virus’s structure, thereby stimulating a broad immune response that could potentially protect against a variety of strains.
The study involved the fusion of hemagglutinin to nanoparticles, which were then used to generate a vaccine. This approach elicited a broader and more robust immune response compared to traditional vaccines. The results showed that these vaccines could provide protection against several different influenza strains, suggesting a significant step toward the development of a universal flu vaccine.
Dr. Karin Bok, a vaccine researcher at NIH, explains, “The use of nanoparticle technology allows us to present the immune system with a more comprehensive picture of the virus, making it more likely to generate a protective response that is effective against multiple strains.” This development represents a significant breakthrough in the fight against mutating viruses.
The potential impact of universal vaccines could be transformative. In the case of influenza, a universal vaccine could potentially eliminate the need for annual vaccinations, which often vary in their effectiveness. Furthermore, the development of such vaccines could significantly enhance global preparedness for future pandemics, ensuring that the world is better equipped to handle emerging diseases.
Conclusion
As the National Institutes of Health (NIH) begins to phase out its COVID-19 research funding, the implications for ongoing studies and future pandemics are far-reaching. By drastically cutting research efforts, the NIH risks leaving a vacuum of knowledge that could hinder the development of effective treatments and vaccines for future outbreaks. The article highlights the NIH’s shift in focus from a long-term research commitment to a more reactive approach, prioritizing immediate needs over sustained investment in scientific understanding.
This shift has significant implications for public health, as it may lead to a loss of momentum in the development of innovative treatments and vaccines. Moreover, the NIH’s decision may be a costly oversight, given the unpredictable nature of pandemics and the potential for future outbreaks. As the scientific community moves forward, it is essential to recognize the importance of long-term research investment in maintaining a robust public health infrastructure.